Red Light Therapy and Oral Mucositis
When you or a loved one is navigating cancer, the focus is often entirely on the "big fight." But the side effects of treatment like oral mucositis can feel like an overwhelming second battle. It is difficult enough to manage the diagnosis without the added burden of painful mouth sores that make eating, drinking, or even speaking a challenge. For parents of young children, seeing their little ones endure this discomfort is especially heartbreaking.
The good news is that we are entering a new era of supportive care. There is a gentle, highly effective therapy called Photobiomodulation (PBM) that is fundamentally changing how we protect patients during treatment.
Why Photobiomodulation is a Vital Shift in Oncology Care
Traditionally, managing oral mucositis meant reacting to pain after it started, using rinses, heavy medications, or even feeding tubes. Red light therapy changes the narrative from reaction to prevention.
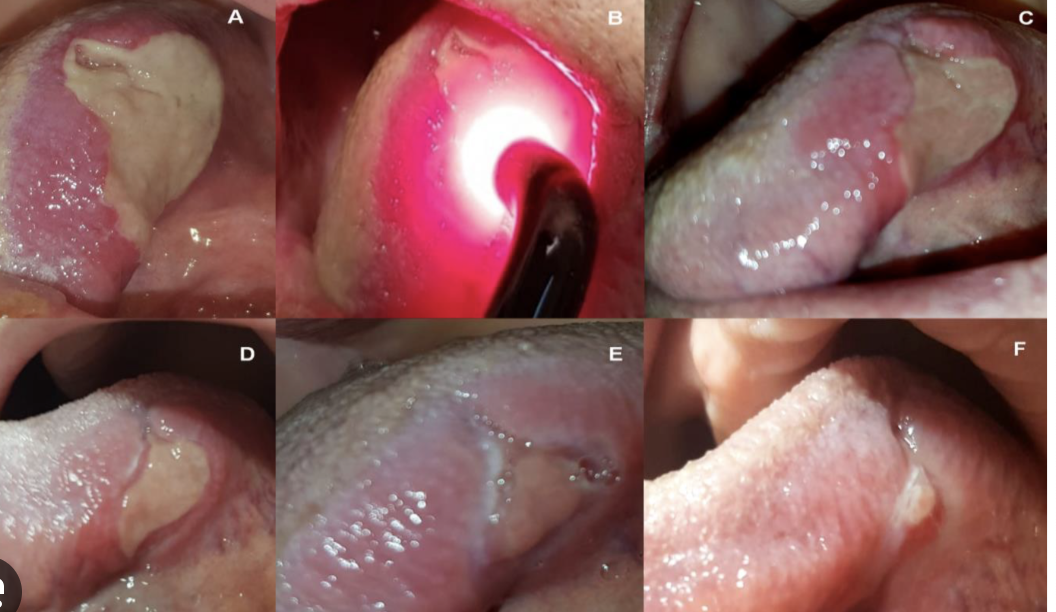
What is PBM? Often called low-level light therapy, PBM uses specific, painless wavelengths of light to "recharge" your cells. It stimulates natural healing and calms inflammation before it takes hold. It isn't invasive, it’s very quick, it doesn't hurt, and it has no known side effects.
The Power of the Evidence
The global medical community is seeing remarkable results. Clinical trials show that PBM can drop the risk of developing severe mucositis from roughly 60% down to less than 10%. Because the evidence is so undeniable, international organizations like MASCC/ISOO, ESMO, and WALT now recommend PBM as a gold standard for patients undergoing head and neck radiation or stem cell transplants.
In short: PBM is no longer a "fringe" idea. It is a proven, science-backed way to keep your treatment plan on track and your quality of life intact.
“The evidence is so strong that international guidelines now recommend PBM for the prevention of oral mucositis in patients undergoing head and neck radiation, chemotherapy, or stem cell transplantation.”
Insurance Coverage
Here’s even more good news: starting in 2026, insurance in the US has begun covering PBM for oral mucositis prevention and management. This is a huge step forward in making this life-changing therapy accessible to everyone who needs it - no more worrying about out-of-pocket costs for this essential care.
Why This Matters
PBM isn’t just another gadget or alternative therapy. It’s a science-backed, patient-centered solution that’s transforming cancer care. By preventing oral mucositis, we’re not just easing pain; we’re helping patients stay on track with their cancer treatment, maintain their nutrition, and preserve their quality of life during an incredibly tough journey.
If you or a loved one is starting cancer treatment, talk to your care team about PBM. It could make all the difference.
Accessing PBM at Your Cancer Center
Are you trying to find out if PBM is offered in your clinic or how you can access it at your cancer center? Let me know, I can help you navigate your options. If you have asked at your cancer center give them my details so we can work together to make this treatment available for more people.
Questions to Ask About Availability of This Treatment
It is so important to feel empowered when walking into these appointments. Since PBM is a relatively new standard of care in some facilities, your clinical team might appreciate you bringing specific, evidence-based questions to the table.
Here is a guide to help you start that conversation and ensure you get the support you deserve:
"Does this facility offer Photobiomodulation (PBM) therapy for the prevention of oral mucositis?"
"If PBM isn't available here yet, do you have a partnership with a nearby center where I could receive these treatments during my radiation/chemo cycle?"
Integrating PBM into Your Treatment Plan
"Based on my specific treatment (e.g., head and neck radiation or high-dose chemotherapy), would I be considered a high-risk candidate for oral mucositis?"
"The MASCC/ISOO guidelines recommend PBM for patients in my situation. Can we look at how to schedule these sessions so they align with my existing appointments?"
"Who on my care team - the oncologist, nurse, or dentist - will be responsible for overseeing the PBM treatments?"
Logistics and Coverage
"Now that insurance coverage for red light therapy has expanded in 2026, can your billing office help me verify that my specific plan covers these preventative sessions?"
"How many sessions per week are typically recommended for my protocol, and how long does each session take?"
Advocacy for the Future
"If the facility doesn't have the equipment yet, would you be open to receiving information from a PBM specialist to see how it might be implemented for patients like me?"
If Photobiomodulation Is Not Currently Available in Your Community
For people who don’t have access to in‑clinic PBM, a home device like the Solasta laser can become a gentle, supportive option rather than feeling like you have no tools at all. The Solasta uses the same healing wavelengths (red and near‑infrared light) that international guidelines recommend in clinical settings for oral mucositis; the difference is simply that you’re using it at home, on the lowest power, for very short, carefully timed sessions to stay within the safe, research‑backed dose range. When I mention Solasta in this context in my blog or teaching, I frame it clearly as “supportive care” rather than a replacement for hospital treatments and always pair it with two promises: first, that you’ll still work closely with your oncology team to decide if light therapy is appropriate for you; and second, that I’ll walk you through exactly how to use it safely - from choosing the gentlest settings, to how many seconds per cheek, to how to avoid the eyes, so you’re getting the potential benefits of PBM without guessing or overdoing it.
Below is a recent video from UK experts on the use of PBM for the prevention of oral mucositis.
Resources
Lavaee F, Rezazadeh F, Amanati A, et al. Efficacy of photobiomodulation for the prevention and treatment of chemotherapy-induced oral mucositis in pediatric patients with hematologic cancers: a randomized clinical trial. BMC Cancer. 2025;25:825.
Wang Q, Oh PS, Jeong HJ. From molecular mechanisms to clinical applications: A comprehensive review of photobiomodulation in cancer treatment. Cancer Photobiology. 2025
Zadik Y, Arany PR, Fregnani ER, et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Supportive Care in Cancer. 2019;27(10):3969-3983.
https://www.frontiersin.org/journals/oral-health/articles/10.3389/froh.2021.689386/full
https://healthtechnology.wales/wp-content/uploads/2022/05/EAR044-PBM-FINAL.pdf
https://static.cigna.com/assets/chcp/pdf/coveragePolicies/medical/cpg030_laser_therapy.pdf
https://www.nature.com/articles/s41598-023-47529-3
https://www.ncbi.nlm.nih.gov/books/NBK587328/
https://www.tandfonline.com/doi/full/10.2217/fon-2019-0461
https://www.sciencedirect.com/science/article/pii/S1011134425000181
https://pmc.ncbi.nlm.nih.gov/articles/PMC10456364/
https://www.journalslibrary.nihr.ac.uk/hta/UWNB3375
https://pmc.ncbi.nlm.nih.gov/articles/PMC7409159/
https://www.sciencedirect.com/science/article/pii/S0360301624016237