Red Light Therapy for Male Fertility: Improving Sperm Health and Motility
Working with your body's natural design is one of the most empowering steps you can take on the path to fatherhood. When a couple faces challenges conceiving, it’s easy for the conversation to feel stressful. But here’s the reality: in about half of all cases, male factors are part of the story, and that is actually a great opportunity for action. It means there are clear, concrete steps you can take to support your own health and your family’s future. It’s also important to understand that up to 10% of male factor infertility cases are caused by potentially life-threatening medical conditions - but most providers simply recommend supplements and ICSI. But just like our cycles give us insights into our overall health so does sperm. IVF can miss out on female and male underlying health conditions as there is usually no root cause investigations into why something is ‘off’.
Most men find the best success by focusing on three main pillars:
1. Embracing the 74-Day Window
Sperm health isn't permanent; it’s a cycle. It takes about 74 days for new sperm to develop, which means every few months, you have a fresh opportunity. Small, consistent lifestyle changes - like prioritizing sleep, choosing breathable clothing, and swapping the hot tub for a cool shower - give your body the environment it needs to produce its best work. It’s not about perfection; it’s about giving your system a better "workspace."
2. Teamwork with Restorative Medicine
Working with a urologist or a fertility specialist doesn't mean you’re "broken." It’s about fine-tuning the engine. Whether it’s balancing hormones, checking for physical blockages, or adding targeted antioxidants medical care helps identify the "why" behind the struggle.
For many couples - particularly those who hold moral or religious convictions, such as Catholic families, the goal is to keep conception within the marital act. This is where "Restorative Medicine" shines. It focuses on healing and working with the body’s design rather than bypassing it through more invasive techniques. RRM investigates the root cause of your fertility issues so you’re creating the healthiest sperm possible - not simply injecting a slow swimmer into the egg.
3. A Gentle "Nudge" with Light
This brings us to one of the most exciting tools emerging today: Photobiomodulation (PBM) - red light therapy. It’s essentially using specific wavelengths of red and near-infrared light to support cellular energy. The goal isn't to "blast" your system, but to offer it a gentle nudge of support.
This little ‘nudge’ of light can improve motility significantly within an hour.
Order your Solasta laser here and receive your personalized male fertility protocol.
The Inner Engine: What the Research Shows
Recent studies have looked closely at how PBM interacts with the very "factory" of male fertility. Research suggests that these gentle wavelengths can have a targeted effect on the specific cells responsible for life:
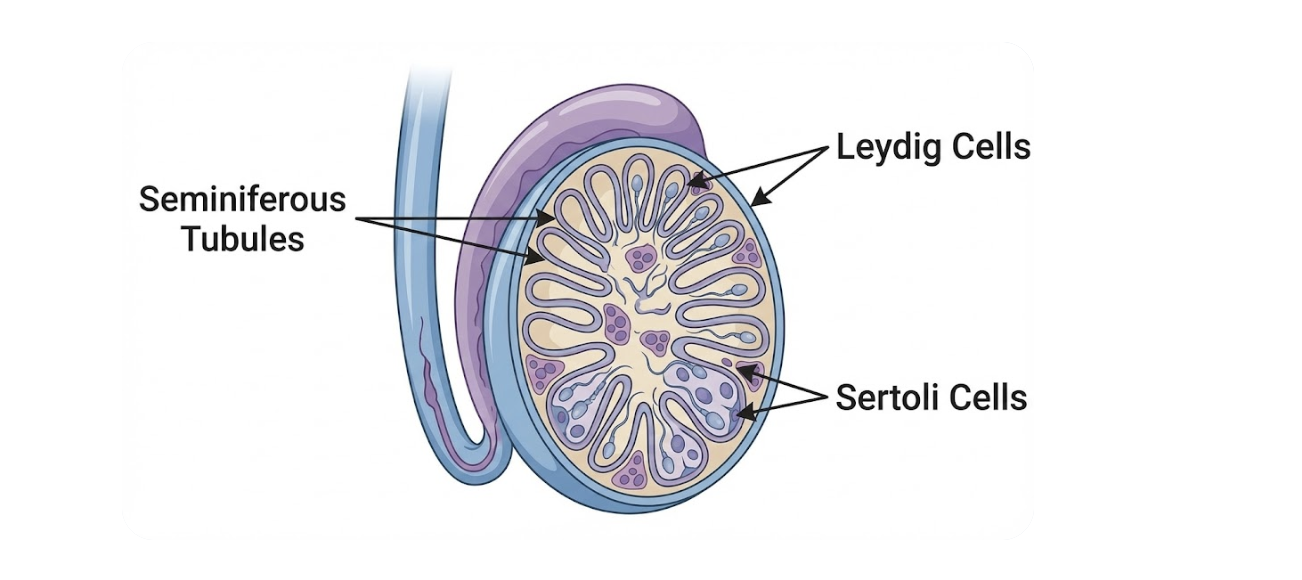
Sertoli & Leydig Cells: These are your "nurse" cells and your "hormone factories." PBM has been shown to support Sertoli cells as they nourish developing sperm and maintain the blood-testis barrier. It also supports Leydig cells, the powerhouses that produce the testosterone necessary for the whole process to move forward.
Seminiferous Tubules & Germ Cells: The seminiferous tubules are the actual structures where sperm is born. Light therapy helps maintain the integrity of these tubules, creating a healthy "home" for germ cells - the precursor cells that eventually divide and mature into healthy sperm. By reducing oxidative stress in these areas, PBM helps ensure that the division process stays on track.
Diagram of seminiferous tubules, leydig cells and sertoli cells.
The "Upstream" Protocol: Why We Start Small
If you’re using a laser protocol, the logic is simple: I follow the map of the body. I don’t start at the destination; the initial goal is to clear the path first. This follows a medical principle called "proximal priority" - treating the areas "upstream" to support the local target.
Step 1: The Core. We start near the upper chest and belly. Think of this as clearing the "highways" of the blood and lymph systems. When circulation is moving freely from the heart downward, everything else functions better.
Step 2: The Gateway. Next, we move to the hips and lower back (sacrum). This area houses the nerves and drainage pathways that serve the pelvis. By supporting these "gateways," we ensure the reproductive organs have the nerve support and circulation they need.
Step 3: The Target. Finally, we move to the reproductive area itself.
Does Red Light Therapy for Male Infertility Work?
Overall yes - with the right dosage, timing and wavelengths is can improve male fertility.
If you like to geek out over the science here’s what scientists have found.
Human sperm (in vitro) – how much did things improve?
1. 810 nm near‑infrared PBM on low‑motility sperm
· In asthenozoospermic men, 810 nm PBM increased progressive motility by roughly 15–25% compared with the same samples before light (example: from about 30% to around 36 - 38% progressive).
· Total motile sperm also rose by a similar margin (about a 10–20% relative increase), without any measurable rise in DNA fragmentation or loss of membrane integrity at 60 minutes after exposure.
In men with sluggish sperm, a single low‑dose 810 nm PBM session made more sperm swim forward, roughly adding an extra 15 - 25% progressive swimmers, without hurting their DNA in the short term.
2. 650 nm red PBM on low‑motility sperm
· In a 650 nm study, total motility in low‑motility samples increased by about 10 - 15 percentage points after PBM (for example, from the low 30s up into the mid‑40s).
· Immotile sperm dropped substantially, by about 20–25% relative to baseline—meaning more sperm were at least moving after light exposure.
· Chromatin (DNA packaging) quality remained stable; they didn’t see a spike in “damaged” DNA.
With red light at 650 nm, more sperm woke up and started moving - roughly one in five previously ‘dead still’ sperm became motile - with no sign that their DNA packaging got worse.
3. Laser/LED PBM on normal donor sperm
· At the “sweet spot” dose, progressive motility rose by roughly 20 - 30% compared with untreated controls over the next 45–60 minutes.
· When the dose was tripled, the benefit almost vanished - motility dropped back close to control values.
At the right dose, PBM gave sperm a 20 - 30% boost in forward swimming; at three times that dose, the boost disappeared - clear proof that more light is not always better.
Animal in‑vivo – how much did PBM rescue damaged testes?
1. Busulfan‑damaged mice (chemotherapy injury)
PBM to the testes:
· Sperm count recovered to about 70 - 80% of normal vs. much lower levels in untreated chemo mice (some busulfan groups sat closer to 30–40% of normal).
· Testosterone levels climbed by around 30 - 40% compared with busulfan‑only animals.
· Markers of oxidative stress (ROS and MDA) fell by roughly 25 - 40%, while antioxidant markers and ATP went up by similar margins.
With a tiny dose of PBM, chemo‑injured mice went from ‘almost no sperm’ toward roughly three‑quarters of normal sperm counts, and their testosterone and antioxidant defenses rose by about one‑third compared with untreated chemotherapy animals.
2. Busulfan + heat damage vs. PBM
In the combined busulfan + scrotal‑heat model:
· PBM raised sperm counts by roughly 2 - 3× compared with the injured animals that didn’t get the light.
· Progressive motility improved by around 20 - 30 percentage points (for example, from ~10% up to ~30–40%).
· Testicular volume and cell counts (spermatogonia, spermatocytes) increased by about 30–50% vs. untreated injury.
In mice whose testes were hit with chemo and heat, adding PBM multiplied sperm counts by two to three times and bumped forward swimmers by about 20 - 30 percentage points, while the testes themselves literally grew back closer to normal size.
3. Heat‑only (transient scrotal hyperthermia)
In transient heat injury models:
· PBM‑treated mice regained near‑normal sperm counts about 1 - 2 weeks faster than heat‑only mice.
· Final sperm counts and motility in the PBM group were typically 20 - 30% higher than in heat‑only animals at matched time points.
After a one‑time overheat, the PBM group’s sperm bounced back a week or two faster, ending up with roughly 20 - 30% more sperm and better motility than the no‑light group at the same time point.
Can Red Light Therapy Harm Sperm?
So far, in controlled settings:
Human semen studies at low doses show no significant rise in DNA fragmentation and no drop in viability at 30 - 60 minutes after PBM.
When the dose was pushed higher: Motility benefits flattened or disappeared (up to ~0% net gain compared to controls), but clear, immediate DNA damage was not reported in those short‑term studies.
In animal models, an appropriate dose markedly improved spermatogenesis, while higher doses showed weaker benefits and hints of the typical PBM biphasic response (too much stimulation becomes counterproductive).
“At the low doses used in lab and animal studies, PBM has improved sperm motility, counts, and even testosterone by anything from 15 - 30% in humans to 2 - 3× in damaged mice, without clear short‑term DNA harm. But when researchers pushed the light dose higher, the benefits faded - another reminder that with sperm and testes, less light, used consistently, is safer and more effective than ‘more, more, more.’”
Is My Red Light Panel Helping?
If you’re casually standing in front of a red‑light panel, most of that light is absorbed by your skin and outer tissue; only a small fraction reaches the actual sperm factory. Short, moderate sessions are unlikely to do much to sperm one way or the other, but very long, very hot exposures - especially day after day could heat the testes and quietly work against sperm quality. That’s why my protocol uses brief, low‑dose, targeted sessions, rather than parking yourself in front of a panel and hoping for the best.
Safety
If you have a history of testicular cancer, a new lump, sudden pain or swelling, or very abnormal semen tests, don’t start PBM on your own. See a urologist first and only use light therapy as part of a plan they approve.
A Whisper, Not a Shout
It’s important to remember that when it comes to reproductive health, less is often more. Sperm are incredibly sensitive to heat and stress. That is why this protocol uses a "low and slow" approach. We’re talking about low level laser therapy (LLLT) not my ‘big’ laser I have in my office.
I don't use high-intensity light or long sessions. Instead, I use a pulsed, low-power setting for just a minute or two per site. We move the device in soft, light circles rather than holding it on one spot. We aren't trying to force the body to do something it isn't ready for; we are simply providing a tiny spark of light to help the cells' "batteries" (the mitochondria) work a little more efficiently.
Supporting fertility is a marathon, not a sprint. By combining lifestyle, restorative medical care, and gentle supportive technologies, you are doing more than just trying to conceive - you are building a foundation of health for yourself and your future child. You’re working with your body to do what a healthy body is supposed to do.
The hand-held Solasta laser uses a combination of red (650 nm) and near‑infrared (808 nm) light, which closely matches the wavelengths used in many of the human and lab studies on sperm health and male fertility. In those studies, near‑infrared around 800 - 810 nm has been especially promising for supporting sperm motility and mitochondrial energy, while red light at similar wavelengths has also been explored at careful, low doses. Because the Solasta laser offers three power settings, we can mimic those protocols by using different power levels on different areas of the body. This lets us stay within the gentle, low‑energy ranges that showed benefit in studies, while tailoring intensity to each body area instead of using a “one‑size‑fits‑all” setting.
Tracy
Resources:
https://blog.tracydonegan.org/blog/is-testosterone-therapy-harming-your-chances-of-conceiving
https://blog.tracydonegan.org/blog/nighttime-light-is-harming-mens-reproductive-health
Zupin P, Ottaviani G, Vuerich R, et al. Photobiomodulation with 810 nm wavelengths improves human sperm motility. Photobiomodul Photomed Laser Surg. 2020;38(4):220‑228.
Karu C, et al. Sperm motility is enhanced by low level laser and light emitting diode light. Lasers Med Sci. 2018;33(5):1085‑1092.
Kouris S, et al. Efficacy and safety of visible and near‑infrared photobiomodulation on human asthenozoospermic semen: wavelength‑dependent regulation of nitric oxide and ATP. Biology (Basel). 2025;14(5)
https://pubmed.ncbi.nlm.nih.gov/32301671/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11538380/
https://pubmed.ncbi.nlm.nih.gov/36610824/
https://pmc.ncbi.nlm.nih.gov/articles/PMC6062680/
https://atm.amegroups.org/article/view/16034/html
https://pubmed.ncbi.nlm.nih.gov/33825170/
https://pmc.ncbi.nlm.nih.gov/articles/PMC12411876/
https://www.sciencedirect.com/science/article/abs/pii/S0024320520305154