The Ultimate Guide to Red Light Therapy for Women’s Pelvic & Vaginal Health
For years, women have been reduced to a body part. The entire conversation around vaginal and pelvic devices has been dominated by marketing that fixates on “tightness” and “rejuvenation,” as if a woman’s worth lives between her legs. What consistently gets overlooked are the real, life-interrupting issues that matter: pelvic pain, pelvic-floor dysfunction, GSM, vulvo-vaginal atrophy, continence, comfort, and a woman’s actual quality of life. You don’t have to look far to find examples of what I’m talking about so I’ll spare you the irritation.
This emphasis on aesthetics and “youthfulness” leaves out a large group of women living with vulvodynia, pudendal neuralgia, genitourinary syndrome of menopause, or the lasting effects of oncology treatments. Their needs are rooted in finding comfort and healing not in looking or feeling younger. This guide was written for them.
What’s Going On Down There?
Estrogen, lubrication, and why tissues feel so different
When estrogen drops (perimenopause, menopause, postpartum, or after certain cancer treatments), the vaginal tissue literally changes shape and behavior. Low estrogen affect this part of your body in the following ways:
The inner tissues of the vagina (mucosa) gets thinner and more delicate (this can also affect the clitoris and vulva).
There’s less glycogen for healthy lactobacilli to feed on, so the microbiome shifts and pH creeps up which can make infections more common.
Blood flow, collagen, and elasticity all take a hit.
On the ground, that looks like: less natural lubrication with arousal, more burning or “sandpaper” feelings with friction, and a higher chance of micro‑tears and infections. It is not “in your head” or a sign you’re not attracted to your partner; the tissue itself is less plump, less slippery, and less protected.
Why the mucosal layer is such a good target for light
The nice thing about vulvovaginal tissue is that it’s thin, vascular, and full of mitochondria and collagen‑making cells. That makes it a very responsive target for light, especially when light is delivered right where it’s needed.
When an appropriate pelvic wand is in direct contact with the mucosa:
Red and near‑infrared light only have to travel through a very thin epithelial layer to reach the basal cells, small blood vessels, and connective tissue underneath.
There’s very little loss from air gaps, clothing, or layers of fat and muscle, compared with shining a big panel at the lower belly or thighs.
That direct contact is why purpose‑built wands can do things panels and general wearables simply can’t for GSM, vulvodynia, or post‑radiation tissue. Panels are great for general wellness and superficial pain, but they are not a substitute for intravaginal or very close‑contact light when the target is the vaginal epithelium and superficial nerve endings.
Significantly reduced pain in 2 weeks.
Almost pain free at 3 months.
What light is actually doing down there
At the cellular level, red and near‑infrared light are absorbed by enzymes in the mitochondria (often described as cytochrome c oxidase), which helps cells make more energy and releases signaling molecules like nitric oxide. Over time, this can:
Improve microcirculation and capillary density (better blood flow and oxygen delivery).
Support collagen and elastin production in the lamina propria (more thickness and flexibility).
Calm some inflammatory signaling so tissues and nerves are less “angry” and reactive.
For a woman who’s low on estrogen, that can translate into:
A lining that’s a bit thicker and more resilient instead of paper‑thin.
Better ability to hold moisture and respond to arousal with engorgement and lubrication.
Less burning and friction pain when there is touch, a finger, a speculum, or a partner.
Light does not replace estrogen where hormone therapy is indicated, but it can be a helpful local support for tissue quality and comfort, especially for women who can’t or don’t want to use hormones, or who are still symptomatic despite them.
Who This May Help, and When to Use Caution
Pelvic photobiomoduation is not a universal solution. Women come with different histories, sensitivities, and goals, which is why I take such a detailed health history and write the protocol based on your unique needs.
Women who may benefit include those navigating GSM, whether related to menopause or low-estrogen states. Symptoms such as dryness, burning, irritation, painful sex, and recurrent infections have been explored in research using red and near-infrared wavelengths, particularly 630 - 660 nm red and around 830 nm NIR.
Women with mild to moderate chronic pelvic pain or pelvic-floor dysfunction may also find gentle support. This might include tension-related discomfort, bladder irritation, post childbirth tenderness, or lingering postpartum sensitivity once they have been medically cleared.
Those dealing with recurrent vulvovaginal infections may benefit from light therapy as an adjunct to medical care, particularly blue and red light used alongside clinician-guided treatment.
Certain situations require specialist supervision rather than a DIY approach. Vulvodynia and pudendal neuralgia often involve extreme sensitivity to pressure, heat, and even light touch. Even wearing underwear can hurt. A “gentle” device may still be overwhelming without expert care. Women recovering from pelvic radiation, chemotherapy, or surgery should work directly with their oncology and pelvic-health teams, as tissues may be fragile or easily irritated. Significant prolapse or a complex surgical history is best approached as a team effort.
Red light therapy is not appropriate without medical advice when there is unexplained vaginal bleeding, suspected or active pelvic cancer, acute pelvic infection, fever, or systemic illness.
Safety First, and Why Ablative Lasers Aren’t Included
Red light therapy for the vagina should feel supportive, not risky. Starting slowly, prioritizing comfort, and stopping immediately if pain, burning, strange discharge or bleeding occur are essential safety measures. Women with hormone-sensitive cancers, complex surgical histories, or implanted devices should always consult their medical team first. This guide focuses only on non-ablative, low-level light therapies, such as LEDs and low-level lasers used for photobiomodulation. These gently modulate cellular activity without burning or destroying tissue. They reflect the evidence described in clinical research such as the Lanzafame and de la Torre rationale for PBM in GSM. Ablative and fractional vaginal lasers operate very differently. They use high energy to intentionally injure or vaporize tissue, are associated with regulatory concerns, and are not designed for at-home use. Because their mechanisms, risks, and oversight requirements differ completely, they are not part of this consumer-focused guide.
Comparing Common Pelvic Light Therapy Devices
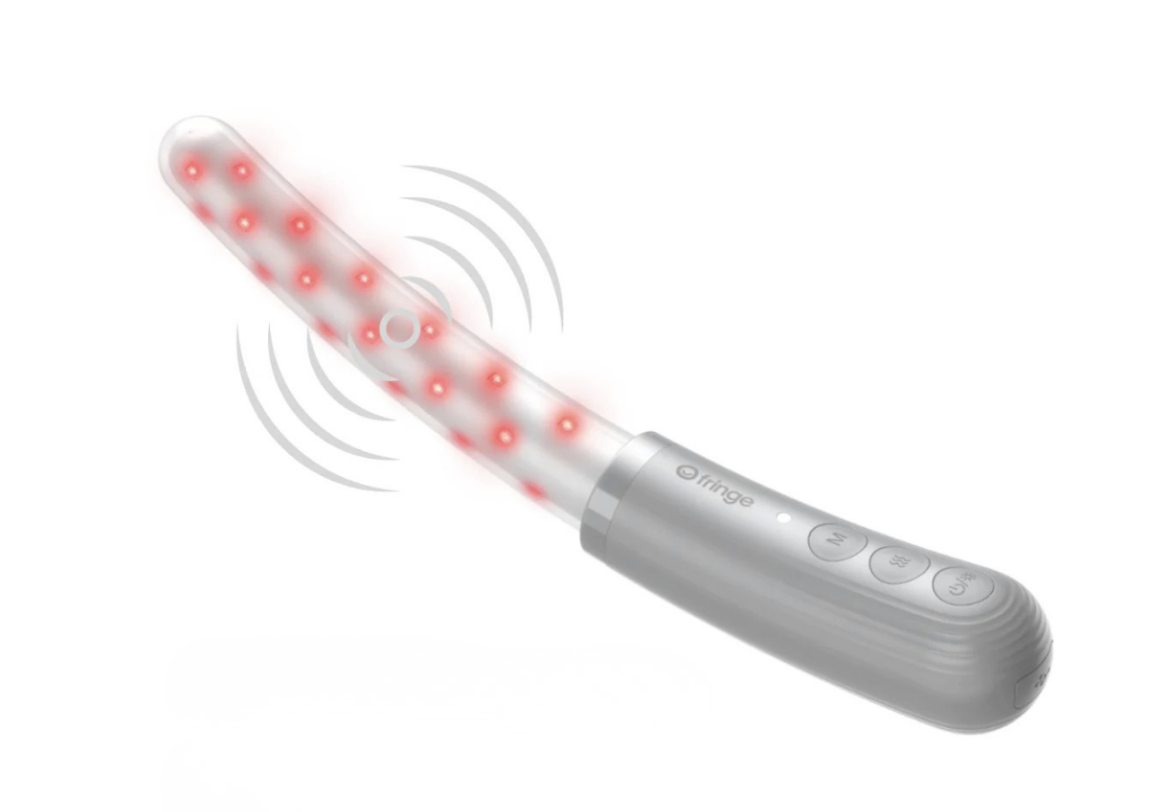
Fringe Heals Therapy Wand: 630 nm red, 830 nm near-infrared, and 415 nm blue. Non-thermal, gentle, wireless, and made of soft medical-grade silicone. Designed to support pelvic pain, continence, and vaginal microbiome health. (I also use it with fertility clients for egg quality).
Chroma Purple Wand: 405 - 420 nm violet, approximately 680 nm red, and approximately 760 nm NIR. Corded, rigid, and often becomes warm or hot in use. It is marketed toward rejuvenation and broad wellness claims.
Photonic Feminine Health Light and Amazon: 650 nm red and 477 nm blue. Battery-powered with possible warmth. No NIR lights for deep penetration. Rigid design with optional vibration.
Devices such as JoyLux and Issviva are not included here because they lack near-infrared outside of Canada, use very few LEDs, and are often described as uncomfortably warm. Their positioning leans more toward thermal rejuvenation rather than true multi-wavelength pelvic photobiomodulation.
These are posts from women on red light therapy groups - sharing their experiences of vaginal red light therapy.
Because the posterior vaginal fornix is only a couple of centimeters across in most women, slimmer, tapered wands are usually easier to position comfortably near this area than short, thick, rigid designs.
What the Research Says About Effective Wavelengths
Studies focus on specific wavelengths for pelvic tissues. Red light in the 630 - 660 nm range and near-infrared around 800 - 830 nm support blood flow, mitochondrial activity, collagen production, and improvements in dryness and pain. The Fringe Wand wavelengths align closely with this research.
Blue light around 415 nm is being studied for recurrent yeast infections, and early findings indicate potential benefit when used alongside standard medical care. The Fringe wand offers blue light in that range. The Photonic wand’s 477 nm blue is further from what current protocols reference. This doesn’t imply it is unsafe; it simply means evidence is more preliminary.
Pelvic Health Issues Worth Highlighting
Women with vulvodynia or pudendal neuralgia often experience allodynia, burning, or severe sensitivity. Rigid devices that become warm can intensify symptoms, whereas softer, non-thermal designs with moderate irradiance are more compatible with their needs.
After oncology treatments, women may face atrophy, scarring, and extreme tissue fragility. The PBM literature suggests a potential role for non-thermal red and NIR light in GSM following cancer treatments, but always with oncology oversight.
GSM deserves specific attention. Symptoms such as dryness, burning, and painful sex are often linked to microcirculatory and mitochondrial changes. PBM targeted at 630–660 nm red and 830 nm NIR aligns well with what the research has found.
Why Device Design Matters for Sensitive Users
Women healing from vulvodynia, pudendal neuralgia, severe GSM/VVA, or post-oncology treatment often need devices that stay cool, use soft and flexible materials, and operate without cords that restrict comfortable positioning. Fringe offers these features. In contrast, the rigid, corded, heat-prone design of the Chroma wand makes it less suitable for women with significant sensitivity or tissue fragility.
Why LED Panels and Wearables Are Not Enough for Pelvic Health
LED panels and wearable red light devices are excellent for skin, joints, and general wellness, but they cannot deliver targeted, direct-contact dosing to pelvic tissues. Light scatters and weakens significantly before reaching the deeper structures involved in GSM, neuropathic pain, or recurring infections. These tools are valuable as external adjuncts but cannot replace a direct-contact device for vulvovaginal applications.
Emotional Wellbeing, Intimacy, and Relationships
Pelvic pain and GSM affect far more than the body. They influence confidence, self-image, emotions, and intimate relationships. Many women describe avoiding sex because of fear of pain, feeling broken, or worrying about their partner’s frustration. These feelings are common and understandable. They are not personal failures.
A wand will not repair a relationship, but easing physical discomfort often removes a significant emotional barrier. Improved lubrication, less burning, and reduced tightness create space for safer, more hopeful exploration and hopefully a return to intimacy. This is one of the reasons society’s obsession with ‘tightness’ or ‘claims that it will leave you feeling like you’re in your 20s again’ sets women up for disappointment.
Does Vaginal Red Light Therapy Work?
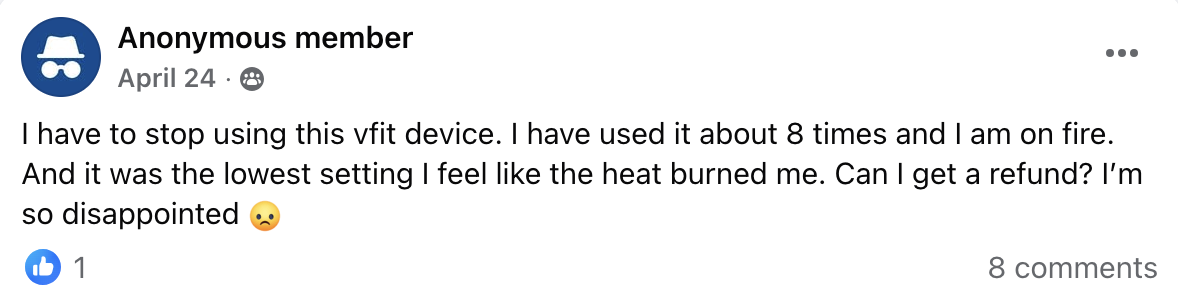
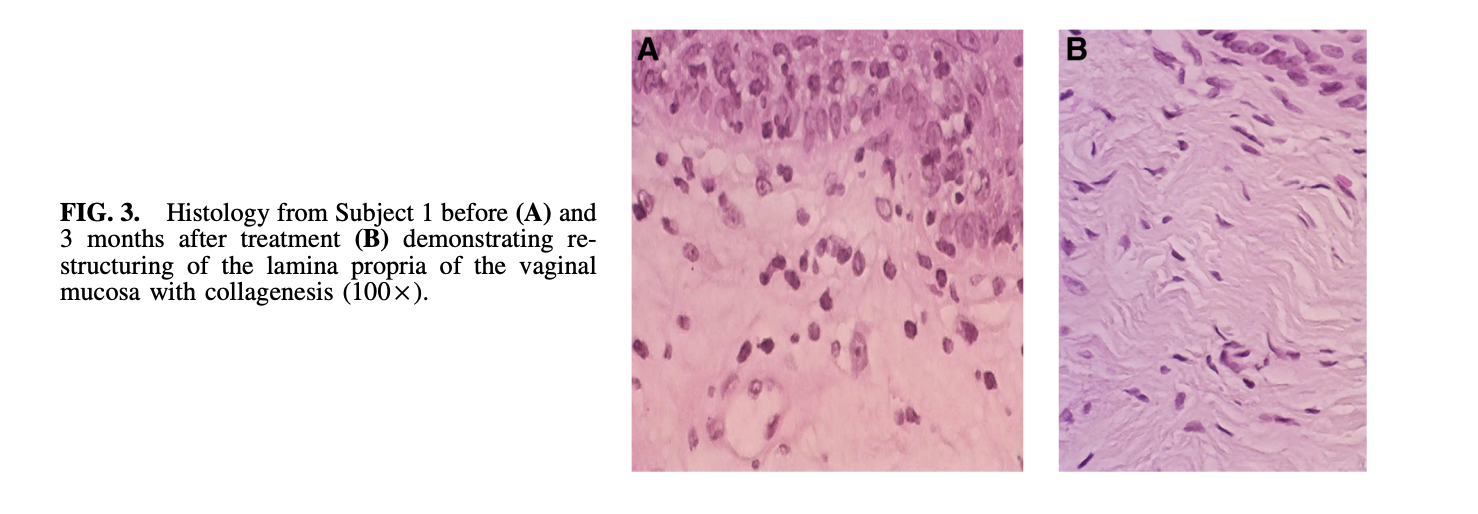
Below are histology images of before and after effects of using specific red light wavelengths on vaginal tissues. Histology is the microscopic study of body tissues, how cells are arranged, how thick a tissue layer is, and how healthy or damaged it looks. In research, small samples of tissue are processed, stained and then examined under a microscope to see changes in structure, blood vessels, collagen, nerves or inflammation.
In this context “histology” means actual tissue‑level changes (for example in the vaginal lining, connective tissue or blood vessels), not just how things feel subjectively. The images below are from a device that includes NIR (in the USA only the Fringe Wand includes NIR (near infra-red).
“My pain (pudendal neuralgia) went from a 10 down to 4 - even snug underwear hurt - and that was only two weeks after starting your protocol.”
Patient 1
Before treatment:
The vaginal lining is thin, dry, and fragile, with poor blood supply and little natural moisture. This kind of tissue can feel sore and tear easily.
3 months after PBM:
The lining is thicker and stronger, with more living cells, better blood flow, and more natural moisture. The tissue now looks plumper and healthier, better able to stretch without pain (this device has NIR).
Patient 2
Before treatment:
The support layer under the surface is weak and not well organized. There are few blood vessels feeding the tissue nutrients and oxygen.
3 months after PBM:
This layer looks denser and more organized, with lots more tiny blood vessels. This means better nourishment and healing for the vaginal tissue.
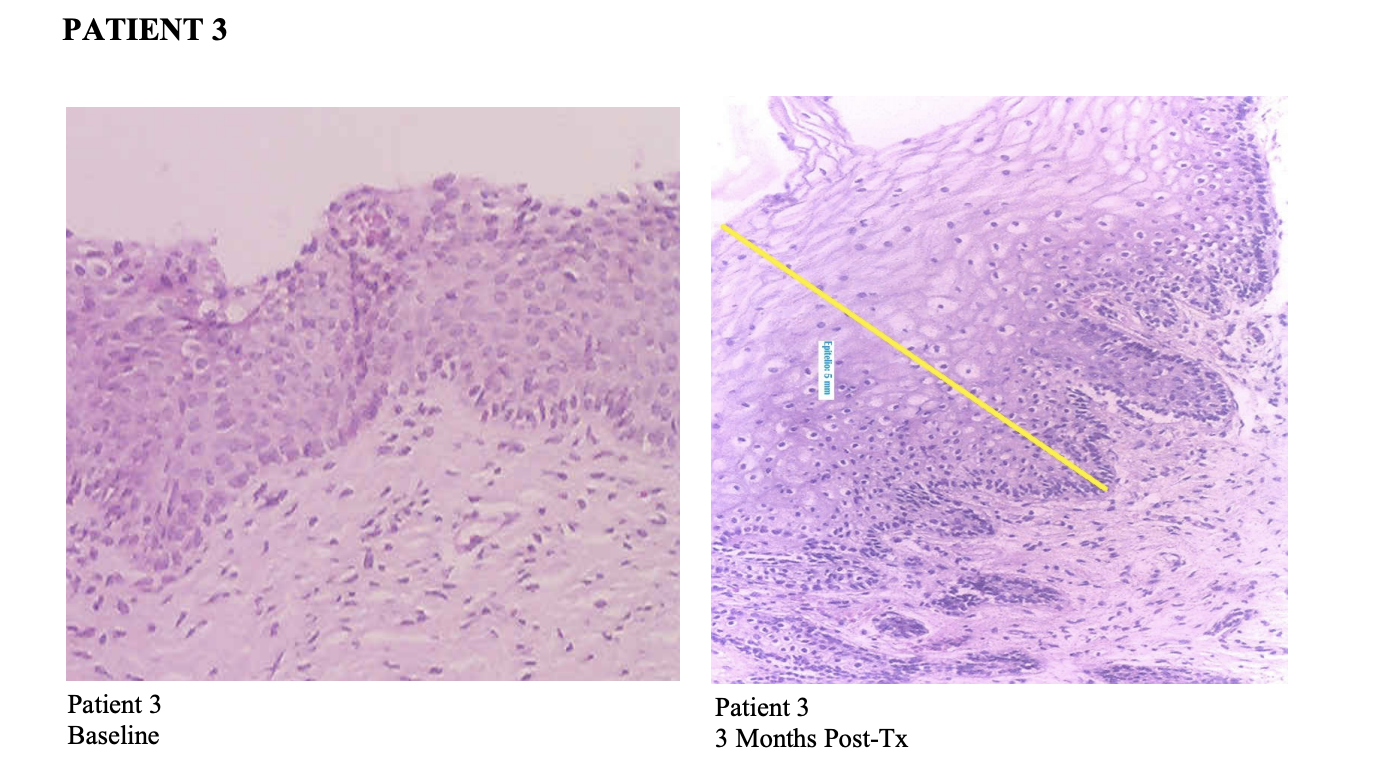
Patient 3
Before treatment:
The surface skin is quite thin and low in glycogen (the “fuel” that helps keep the vagina moist and healthy).
3 months after PBM:
The surface is clearly thicker and holds more glycogen. This usually means better lubrication, more comfort, and stronger protection against irritation.
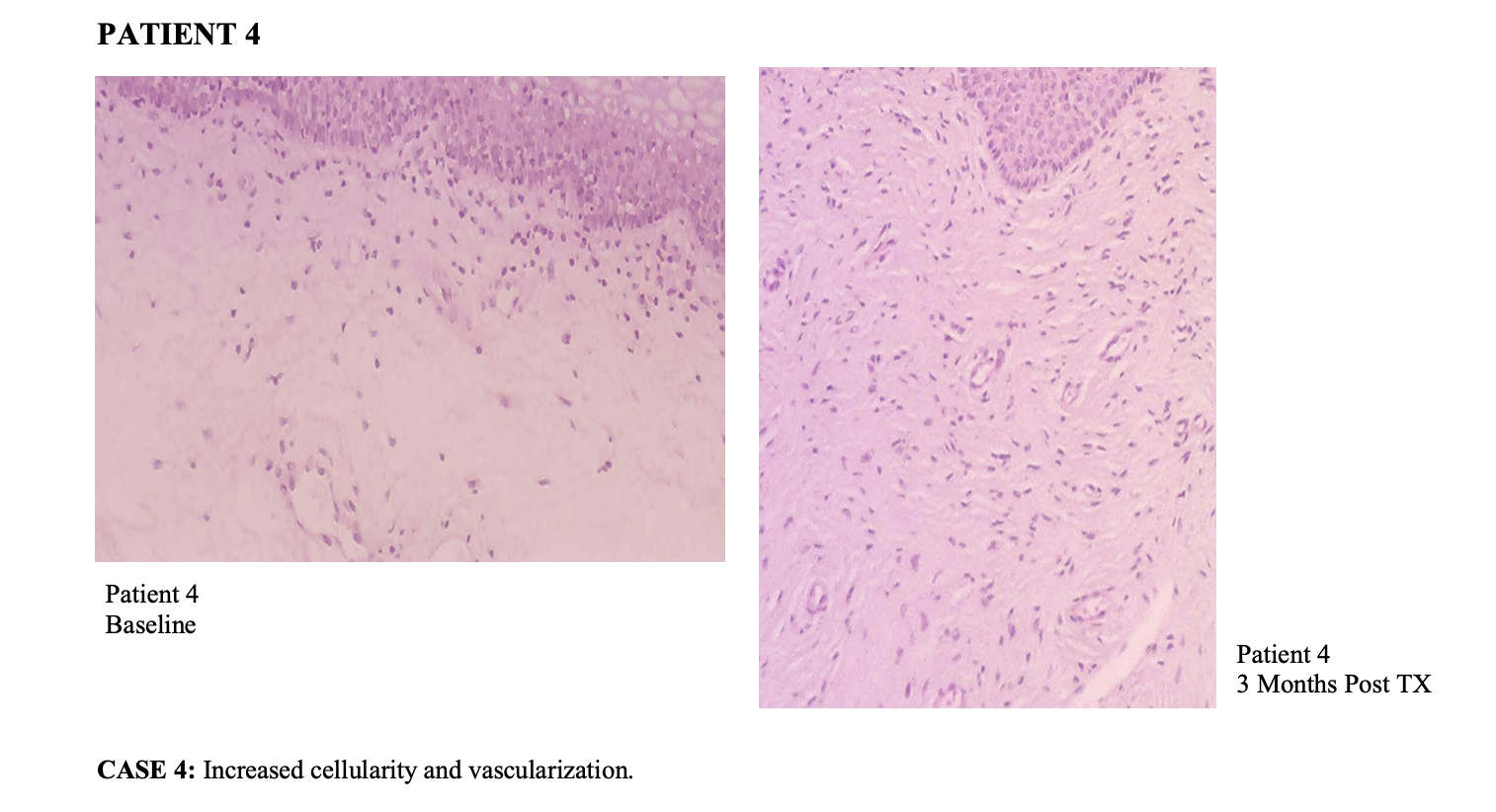
Patient 4
Before treatment:
The tissue looks pale, with not many cells and limited blood flow.
3 months after PBM:
There are more cells and more small blood vessels throughout the tissue. The whole area looks healthier and better supplied with oxygen and nutrients.
Vaginal/Pelvic Light Therapy Q&A
Is a pelvic light wand safe if I have vulvodynia or pudendal neuralgia?
Possibly, with the right device and professional guidance. Non-thermal, soft, slim devices such as Fringe are most appropriate. Rigid or heat-producing wands are usually not recommended for nerve-driven pain.
Can I use light therapy after breast or gynecologic cancer?
There is emerging evidence that non-thermal red and NIR PBM may help with GSM after cancer treatment. Decisions should be made in collaboration with oncology and gynecology.
How long before I notice changes?
Most women see gradual improvements over several weeks to months. Some clients experience reduced pain within 2 weeks with a conservative sensitive approach. Early changes may include less burning, easier exams, or more comfort with gentle external touch.
What if penetration isn’t possible for me right now?
Light therapy can begin externally or with very shallow use under my guidance. Penetration is not required for progress.
How is this different from a rejuvenation laser?
PBM wands support cellular function without burning tissue. Thermal rejuvenation devices rely on heat or vibration and often lack evidence-aligned wavelengths. Ablative lasers intentionally injure tissue and are not part of this guide.
Can I overdo it?
Yes. PBM follows a biphasic dose response, meaning too much can irritate tissues. Gentle, conservative, consistent dosing is more effective than longer or more frequent sessions.
What if I feel worse afterward?
Stop immediately and consult your professional light therapist. This is your body providing important feedback.
Safety and Softening Meditation
Because pain, guarding, and past experiences live in the nervous system as much as in the muscles, every Fringe wand purchased through my website includes a bonus audio meditation and visualization. This guided track is designed to help women shift out of ‘fight or flight’ and into more of a ‘rest and digest’ state before and during wand use. The focus is on slow breathing, softening the belly and pelvic floor, and creating a sense of safety in the body so tissues are less likely to clamp down the moment anything comes near the vulva or vagina.
Many women find that pairing light therapy with a familiar, soothing audio makes sessions feel less clinical and more like a ritual of care. It can also be a helpful tool for therapists to recommend between visits, especially for patients with a lot of anticipatory anxiety, pelvic guarding, or a history of painful exams and procedures.
The Naysayers
Many women are told that pain, dryness, and embarrassment are just part of getting older or going through menopause. Yet studies of vaginal photobiomodulation show the opposite story: when gentle red and near‑infrared light is brought directly to the vaginal tissues, those tissues can become thicker, better nourished, and more comfortable again, with real improvements in lubrication, pain, and sexual function.
There will always be people who say ‘light inside the body can’t do anything, but that is not what the histology slides or women’s lives are showing. Under the microscope, post‑treatment tissue has more blood vessels, more collagen, and a healthier surface layer; in real life, women report less burning and tearing, more ease with intimacy, and a sense of getting part of themselves back. So if you are living with genitourinary symptoms of menopause or post oncology pain, it is not “all in your head,” and you are not out of options. There is a growing body of evidence - and a growing number of women, showing that when therapeutic light is brought gently inside the vagina, it can support healing at the cellular level and help restore comfort, confidence, and pleasure.
Tracy