Red Light Therapy: A Breakthrough for Hypertension and Pre-Eclampsia
Today, we're exploring an important topic for expectant mothers, especially those at risk of hypertension and/or pre-eclampsia and how red light therapy may be a promising adjunct to current medical care.
Hypertension is high blood pressure in pregnancy and means your blood pressure stays higher than normal after 20 weeks, which can put extra stress on you and your baby. Sometimes this high blood pressure turns into preeclampsia, where there are also signs that the placenta and your organs are under strain, so you and baby need closer monitoring and care
What is Pre-Eclampsia?
Pre-eclampsia is a serious and common pregnancy complication that usually happens after 20 weeks of gestation. It’s usually characterized by high blood pressure and often protein in the urine. This condition can affect various organs and, in severe cases, can be dangerous for both you and your baby. But with proper monitoring and care, most women and their babies do just fine. It may necessitate an earlier than planned birth for your baby which isn’t ideal but at the moment medicine doesn’t have much else to offer. And in some cases moms can develop eclampsia - after birth.
Outside of pregnancy, red and near‑infrared light therapy has been shown to lower blood pressure and improve blood vessel health, in part by helping the body release more nitric oxide, a natural vasodilator. The 670 nm placenta study described below fits into this bigger picture by showing that the same kind of light can also improve nitric‑oxide related signaling directly in pre‑eclamptic placental tissue. At the same time, there are still no clinical trials in pregnant women testing light therapy specifically for high blood pressure or pre‑eclampsia, so this approach is promising but not yet proven in pregnancy.
Hypertension (high blood pressure) is a common sign of preeclampsia.
Symptoms to Watch For
Pre-eclampsia can sometimes be tricky to spot because it might not cause obvious symptoms initially. However, here are some signs to keep an eye on:
Swelling: Sudden swelling of the hands, feet, or face.
Headaches: Severe headaches that don’t go away with usual treatments.
Vision Changes: Blurred vision, seeing spots, or light sensitivity.
Upper Abdominal Pain: Pain just under the ribs on the right side and/or nausea.
Nausea or Vomiting: Especially if it’s sudden and severe.
If you notice any of these symptoms, it’s important to contact your healthcare provider right away.
Who is at Increased Risk?
Certain factors can increase the risk of developing pre-eclampsia. Here’s a rundown of who might be more susceptible:
First-Time Moms: It’s more common in first pregnancies.
History of Pre-Eclampsia: If you had pre-eclampsia in a previous pregnancy, the risk is higher.
Family History: If your mom or sisters had pre-eclampsia, your chances might be higher.
Multiple Pregnancies: Carrying twins, triplets, or more can increase the risk.
Age: Women under 20 or over 40 are at higher risk.
Existing Health Conditions: Conditions like high blood pressure, diabetes, gestational diabetes, kidney disease, and certain autoimmune disorders can increase risk.
Obesity: Being overweight or obese can elevate the risk.
In Vitro Fertilization (IVF): Pregnancies achieved through IVF may have a higher risk of pre-eclampsia.
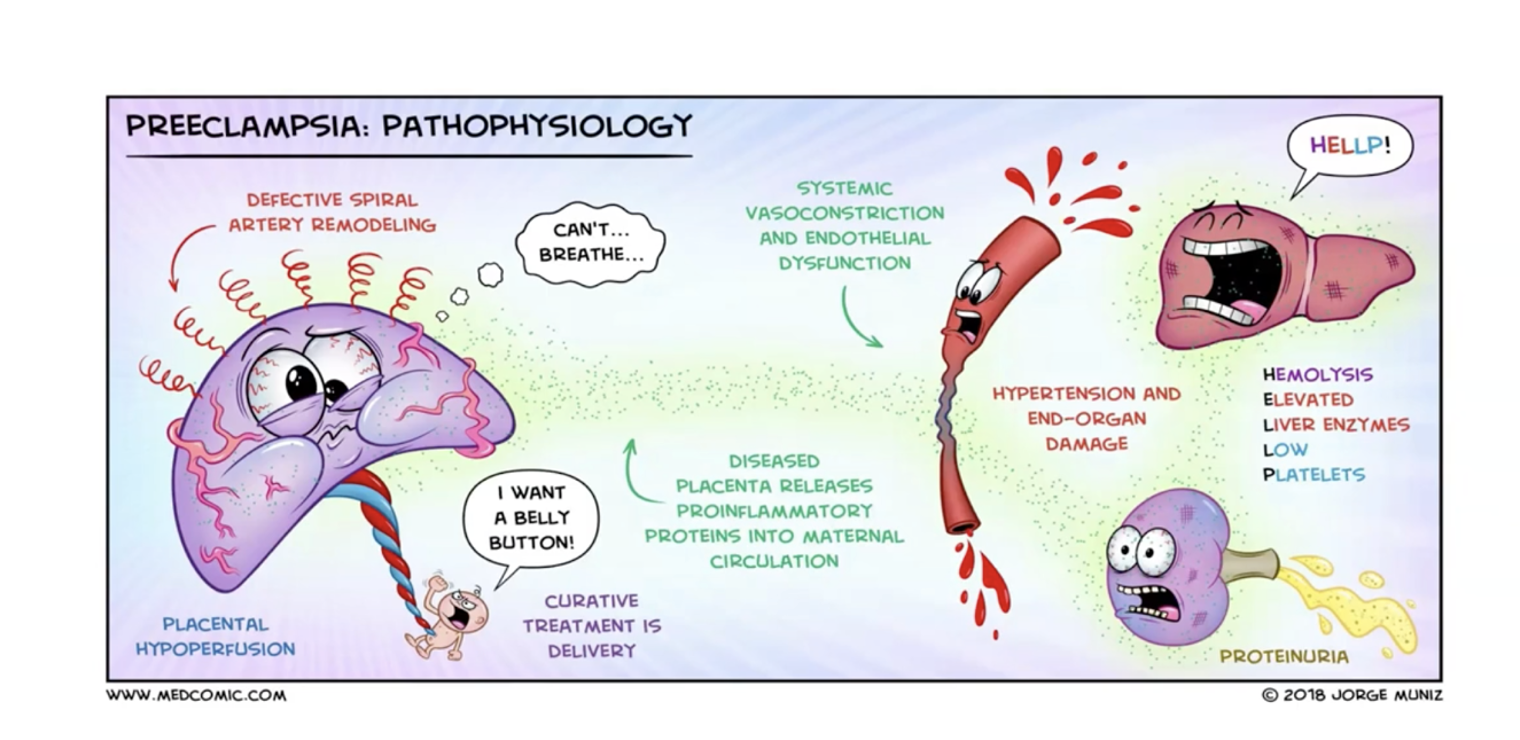
What is going on in the body when a woman develops preeclampsia?
Red Light May Help Your Placenta Work More Effectively By Increasing Nitric Oxide
Preeclampsia happens when the blood vessels in the mom’s body and in the placenta aren’t working properly, so less blood and oxygen get to the baby. A important ‘relaxing’ chemical called nitric oxide is low, and some of the blood tests that should support healthy blood flow to the placenta are out of balance.
The Study: Red Light as an Adjunct Therapy Researchers from the Medical College of Wisconsin explored how red light therapy applied to cells in a lab, specifically at a wavelength of 670 nm (for only 40 seconds), can improve placental health in cases of late-onset pre-eclampsia in samples from placentas of women who had pre-eclampsia. Here’s what they found:
Improved Placental Environment:
Red light therapy reduced harmful oxidative stress markers in the placental extracellular matrix (ECM). This is crucial because a healthier ECM means better support for the growing baby.
Boosted Trophoblast Function:
Trophoblasts are cells that form the outer layer of the placenta and are vital for nutrient and oxygen exchange between mom and baby. The therapy improved their behavior, enhancing their ability to migrate and function properly.
Increased Nitric Oxide (NO):
Nitric Oxide is essential for blood vessel health. It acts as a vasodilator widening blood vessels sending rich oxygenated blood and nutrients to your baby. Red Light Therapy increased NO availability, which helps in maintaining proper blood flow to the placenta. The authors interpret the benefit of 670 nm as releasing additional NO from other internal stores (e.g., nitrosothiols, heme‑NO) rather than ‘fixing broken eNOS’.
Exposure to light reduced cell death and helped the cells involved in placental development move properly again, similar to how they behave in a healthy placenta. How amazing is that! Additionally, shining 670 nm light restored important growth factors to normal levels. This research suggests that using 670 nm light can help repair the damaged environment in the placenta caused by late-onset preeclampsia.
There is currently no research on using photobiomodulation during the first trimester which is when the placenta ‘invades’ the uterine wall and the spiral arteries begin to develop - so we don’t yet know when is the best time to use red light therapy. It’s important to note that this study was on samples from full term placentas not on pregnant women. This lab research suggests 670 nm red light can repair aspects of a damaged placental environment in tissue samples from women with late‑onset pre‑eclampsia, which raises the possibility, but does not yet prove that similar approaches might one day help reduce complications.
Current opinion advises not to place the light over the bump. However there may be other ways to increase your body’s natural production of nitrix oxide. Red light has a systemic effect on the whole body, meaning it’s possible to use the same wavelength on your back or thigh with a skin contact device. Coincidentally this is the same wavelength (670 nm) shown in recent studies to reduce blood glucose levels (15 minutes) and has also been used in Australia directly on preterm babies in the NICU. These findings are from late‑onset cases and may not fully apply to early‑onset pre‑eclampsia. But I think this warrants a discussion with your midwife or OB given the high safety profile of photobiomodulation in research demonstrating no adverse effects when used appropriately.
A 2025 systematic review on PBM for hypertension found that small clinical trials using red/NIR light (mostly 630 - 830 nm, produced average systolic BP reductions of about 10–15 mmHg, along with modest diastolic and heart rate reductions, though the overall certainty of evidence was rated very low due to small, heterogeneous studies.
In one randomized trial of intravascular 660 nm red light therapy in women on endocrine therapy after mastectomy, weekly treatments significantly reduced systolic and diastolic pressures and heart rate compared with controls, suggesting a very real hemodynamic effect even in a high‑risk cardiovascular group.
Animal studies show similar benefits - even in over fed obese mice.
What We Don’t Know Yet
No human trials have tested 670 nm PBM to prevent or treat pre‑eclampsia in pregnant women.
The study used direct lighting of cells and ECM, not by using the light on the upper back or thigh.
First‑trimester use has no data; even the authors highlight that more work, especially in earlier disease and in vivo models, is needed.
As of November 2025 there are no skin contact devices available with 670 nm. However 660 nm is still within the therapeutic window and the NovaaLab pad is one of my favorite devices for multiple home use including postpartum applications. It was also used in the women who had mastectomies with success.
In the research on cardiovascular red light therapy and Nitric Oxide release, the most common wavelengths are around 630 - 670 nm (especially 660/670) and around 800 - 850 nm (especially 808/810 and 850). The Novaa pad has the right wavelength mix (660/850) and wrap form factor, so it is well‑suited for the kind of cardiovascular‑support. However its relatively high surface power means dosing and placement would need to be adjusted carefully for moms (by purchasing using my link I will write a personalised protocol for you - only for this complication of pregnancy. Due to the time and research protocols take to create I have had to limit my protocol work to my own devices (Solasta Laser).
How a "Spotlight" on Your Leg Can Your Body
You might wonder: How does putting light on my leg help anything else? The answer lies in a tiny, hero molecule called Nitric Oxide (NO).
Research (including studies on circulation) suggests that when 670 nm red light hits the muscles in your leg, it triggers the release of Nitric Oxide. Think of NO as a "natural relaxer" for your blood vessels. It helps them open up, allowing blood to flow more smoothly causing less damage to your blood vessels.
Here is the "Why" behind the red light thigh pad:
Local Support: The light helps improve blood flow right where it’s applied. This can be great for leg comfort and helping blood return from your lower body back toward your heart.
Targeted, Not Overwhelming: Unlike some treatments that affect your whole system, this light therapy seems to work locally. This means you get the benefits of better circulation in that area without a sudden, dramatic drop in overall blood pressure.
A Cellular "Hug": It helps the lining of your blood vessels (the endothelium) stay healthy and resilient.
Safety First: The "Golden Rules" for Pregnancy
Because your health and your baby’s safety are the absolute priorities, there are a few things to keep in mind if you’re considering red light:
Always Check with Your OB: Before trying anything new - even something as gentle as light - your doctor needs to give the "all clear." They know your specific case best.
Limb Only, Not the "Bump": Most experts suggest using red light on the limbs (like the thighs) rather than directly on the abdomen. This is mostly out of an abundance of caution, ensuring we support your circulation while leaving the "nursery" undisturbed.
An Extra Tool, Not the Whole Kit: It’s important to remember that red light is a supportive adjunct. It doesn’t replace your aspirin, your doctor’s appointments, or your blood pressure cuff. Think of it as a "gentle helper" that works alongside your main medical plan.
The Bottom Line
We don't have enough data yet to say that red light can prevent or treat preeclampsia - that’s a big job that requires serious medical management. However, we do know red light therapy used properly is a very low-risk way to support your vascular health and local circulation.
If your doctor is on board, a 15-minute "light break" for your legs could be a peaceful way to support your body's natural pathways during this important time.
Note: The NovaaLab pad has not been clinically tested or cleared specifically for preeclampsia or gestational hypertension. Red light therapy may be helpful as an adjunct treatment along side the expert care of your provider. I do NOT recommend using photobiomodulation to manage these dangerous conditions independently.
Potentially, red light therapy could be a preventative adjunct tool for Gestational Diabetes, Pre-Eclampsia and other metabolic disorders of pregnancy given it’s impact on mitochondria and celllular signalling but more research is needed.
If you are at risk of pre-eclampsia, this therapy could offer a non-invasive way to improve placental health and reduce complications alongside the care of your provider.
I’d love to hear your thoughts, is this something you would be interested in discussing with your provider? Are you an OB with an interest in a feasibility study?
Tracy
Resources:
https://pmc.ncbi.nlm.nih.gov/articles/PMC12524357/
https://pubmed.ncbi.nlm.nih.gov/41095798/
https://pubmed.ncbi.nlm.nih.gov/36462596/
https://liebertpub.com/doi/abs/10.1089/photob.2022.0127
https://pubmed.ncbi.nlm.nih.gov/38165554/
This article is for education only and is not medical advice. Red light therapy for high blood pressure or pre‑eclampsia in pregnancy is still experimental and has not been proven in clinical trials. Never start, stop, or change any treatment in pregnancy based on online information alone. Always talk with your midwife or doctor about your individual risk factors, symptoms, and any devices or therapies you are thinking about using.